Addressing Maternal Mortality and Morbidity in the U.S.
This page serves as a repository of information, resources, tools, and evidence-based practices, to help your Healthy Start program use and enhance its educational, care coordination and community mobilization capacities to address the overlapping risk and protective factors that impact both maternal and infant health. The “More” button below each featured resource will take you to additional information and resources.
DefinitionsMaternal mortality: A pregnancy-related death is defined as the death of a woman while pregnant or within one year of the end of a pregnancy – regardless of the outcome, duration or site of the pregnancy – from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. Maternal mortality ratio is the number of maternal deaths during a given time period per 100,000 live births during the same time period. (CDC) Severe maternal morbidity (SMM): SMM includes unexpected outcomes of labor and delivery that result in significant short- or long-term consequences to a woman’s health. (CDC) |
Staff Meeting Training Package: Promoting Women’s Health to Prevent Maternal Mortality
 This Staff Meeting Training Package provides everything you need for a short (under an hour) staff development activity that you can do with your entire Healthy Start team during a staff meeting or other team meeting.
This Staff Meeting Training Package provides everything you need for a short (under an hour) staff development activity that you can do with your entire Healthy Start team during a staff meeting or other team meeting.
The Big Picture: Maternal Mortality in the U.S.
Lost Mothers: Maternal Mortality in the U.S.
This series of podcasts focuses in on maternal mortality in the U.S. and what can be done to prevent maternal deaths. NPR, 2017-18
- To Keep Women From Dying In Childbirth, Look To California
- Focus On Infants During Childbirth Leaves U.S. Moms In Danger
- Black Mothers Keep Dying After Giving Birth. Shalon Irving’s Story Explains Why
- For Every Woman Who Dies In Childbirth In The U.S., 70 More Come Close
- Many Nurses Lack Knowledge Of Health Risks To Mothers After Childbirth
- Redesigning Maternal Care: OB-GYNs Are Urged to See New Mothers Sooner And More Often
- Nearly Dying In Childbirth: Why Preventable Complications Are Growing In U.S.
- ‘If You Hemorrhage, Don’t Clean Up’: Advice From Mothers Who Almost Died
- U.S. Has The Worst Rate Of Maternal Deaths In The Developed World
Data and Statistics
CDC’s Pregnancy Mortality Surveillance System
This webpage describes how CDC collects and uses data on pregnancy-related deaths in the U.S., and provides national statistics and trends.
What Works: Health Care Clinical and System Interventions
Alliance for Innovation on Maternal Health (AIM)
This initiative works toward the end goal of eliminating preventable maternal mortality and severe maternal morbidity across the U.S.
What Works: Ensuring Access to Preconception, Prenatal and Postpartum Care
Black Mamas Matter: Advancing the Human Right to Safe and Respectful Maternal Health Care
This toolkit provides an overview of information and resources on Black maternal health and identifies action policymakers can take to address maternal health within human rights and reproductive justice frameworks. Center for Reproductive Rights, 2018
What Works: Continuous Support through Pregnancy and Delivery
Cities turn to doulas to give black babies a better chance at survival
This article highlights how doula support during and after pregnancy leads to healthier babies and healthier outcomes for mothers. Washington Post, 2017
What Works: Raising Awareness/Education of Women and Families
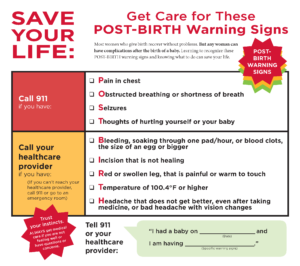
Save Your Life: Get Care for These POST-BIRTH Warning Signs
This handout helps women to recognize post-birth warning signs and tells them who to contact to get the appropriate medical care. Also available in Spanish. Association of Women’s Health, Obstetric, and Neonatal Nurses, 2016